First of all, we note that there are actually two vaccines on the table. The first, RTS,S, is recommended and approved by the WHO while the other, R21, is still undergoing trials. However, while the Federal Ministry of Health has announced that the country has now placed orders for RTS,S, expected to be delivered by April 2024; the NAFDAC has given approval, not to the RTS,S, but to the R21.
The approval given to the R21 will allow it to be used in clinical trial settings in the country. NAFDAC said it had shunned participation in the clinical trials for RTS,S because its touted efficacy of about 30% was simply not attractive enough ab initio.
Speaking extensively on Channels TV, the DG, Prof Moji Adeyeye, emphasised that unlike the case for COVID vaccines, when NAFDAC gave approvals without actually testing the products, the situation will be different this time. During COVID, the WHO had foisted on NAFDAC some novel Protocols, such as “Reliance”, which authorizes it to simply rubber-stamp whatever decision has been announced by the WHO; and “Recognition” (which encourages it to regurgitate statements made by so-called “more matured” Agencies from other countries – where the WHO itself is circumspect of making any statements). This time around there would be clinical trials in Nigeria, and that for R21would be commencing within 6 weeks.
That is some cheering news, for a change!
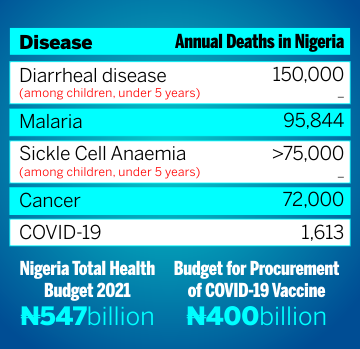
But before we become too engrossed in the subtle battle for supremacy among the malaria vaccines, (and possibly between government Agencies also), we need to examine what exactly is the place of vaccines in managing a disease that reportedly kills about 200,000 Nigerians every year. This figure represents 31.3% of total global mortality attributed to malaria.
Without any doubt, any solution that could dent that horrible figure is to be celebrated and embraced. The search for a useful vaccine for malaria had been on for more than 50 years, and we must congratulate the brilliant researchers for their hard work, doggedness, and at last, a visible result. It is tough enough trying to develop vaccines against viruses and bacteria, a vaccine for malaria is another story entirely. The disease is carried by a parasite involving two hosts – the female anopheles mosquito and humans. The parasite itself has some 5 species that infect humans, each existing in different forms at different stages of their life-cycles. The life cycle begins as sporozoites deposited into human liver, and later moves to the blood (erythrocytic phase) before finally ending up back in the salivary gland of the anopheline mosquitoes, thus perpetuating the cycle. The daunting scientific difficulties involved in trying to get a safe and effective vaccine against this challenge are well enunciated in the literature, for example here and here.
However, a vaccine solution must be justified not only on its own merit, but also on how well it fits in within the framework of holistic malaria management in a country. In particular, it should complement other tools rather than jeopardize them.
Factors determining the merit or otherwise of a vaccine solution include 1) Efficacy - that is the whole point of the tool, anyway – how well does it work? 2) Duration of the efficacy - how long after full dosage before the efficacy wanes and “boosters” become necessary? 3) Target biological endpoint and its relevance - What exactly does it “prevent” – new infections? hospitalizations? (Perhaps we should focus more on identifying and dealing with the risk factors for severe malaria, and stop counting “cases”!). 4) Safety - are the health risks introduced by the intervention justifiable relative to the benefits? 5) the Logistics involved in its procurement, storage, and delivery (for instance the number of doses required for full dosage: the higher this number, the higher the chances of non-full compliance and consequent failure). 6) the Costs of the whole enterprise, and 7) possible Spin-off benefits for other sectors.
As pointed out by DG NAFDAC, the RTS,S vaccine would score very low based on these considerations. Not only is the touted efficacy rather low at 30-40%, it needs to be administered in at least four doses posing considerable programmatic challenges. The duration of this efficacy has been determined to be about only 7 months. Even with possible financial supports (specific for the malaria vaccine, and for a limited period) the (non-negotiable) cost of $3-$4 per dose is not exactly pocket-friendly, especially for an expense that might as well become an annual ritual of 4-5 doses per child.
However, the big issue with the RTS,S is safety. It remains an indelible ugly stain on the WHO, that in the clinical trials for the RTS,S, conducted directly under her auspices, the WHO withheld critical safety signals raised during Phase III trials from African participants in the Phase IV clinical trials. These were: “a ten times higher rate of meningitis, a higher chance of cerebral malaria, and a doubling of deaths from all causes in girls who had received the vaccine and not the placebo.”
Obviously, these are very serious issues indeed. Though the WHO subsequently suggested that the safety issues had been somewhat cleared, many authorities flatly disagreed. In any case, it is rather difficult mending trust so flagrantly breached.
We raise our first pertinent question at this juncture: are the clinical trials to be conducted under the auspices of NAFDAC for the R21 vaccine going to check out for these safety issues also? And how long will it take before the answers will become available? In short, will the NAFDAC be open and transparent in making available to the general public the protocols to be used for these clinical trials? Sadly, up to the present time, access to the Vaccines and Biologics section on NAFDAC’s website remains passworded and unavailable to the general public, unlike those for other categories, viz: Food, Drugs & Medical Devices, Herbals & Cosmetics, Chemicals, Narcotics, and Veterinary.
Clearly, there is need for caution before one exuberantly concludes that the R21 will eventually outperform the RTS,S. This more so, when it is realized that the two vaccines are actually essentially based on the same principle and materials. Both target the pre-erythrocytic phase of malaria, with the key antigen provoking an immune response being the Circumsporozoite Protein (CSP) (secreted by the sporozoites of Plasmodium falciparum), bundled with hepatitis B virus epitopes. The major difference in the two is that the concentration of the CSP is higher in R2,1 than in RTS,S; and both have different adjuvants - materials required to amplify the immune response. RTS,S uses GSK’s AS01 as adjuvant, while R2,1 employs NOVAVAX’s MATRIX-M (same used for their COVID-19 vaccine).
There are other issues with the two vaccines that raise serious concerns. For instance, while it is indeed reasonable that these vaccines should target Plasmodium falciparum which is responsible for as much as 98% of malaria mortality in sub-sahara Africa, it is well known that other species, particularly the Plasmodium vivax could persist in the blood for years, thereby promoting the recurrence of malaria in the absence of any new infection. Even more concerning are results from Kenya suggesting that the RTS,S vaccine could delay the acquisition of the far more robust natural immunity in recipients.
That leads us to the second broad consideration that could justify the incorporation of the vaccine tool into the general holistic management of malaria: How well does it fit in with existing tools?
The available non-immunization approach to malaria management include General environmental sanitation to eliminate stagnant pools of water where mosquitoes could breed - the principal assignment for Environmental Health Officers a few decades ago; use of insecticide treated nets, use of various manners of insecticides or repellants, use of chemical prophylaxis (e.g. “Sunday-Sunday”, Daraprim), and appropriate therapeutics - both herbal and synthetics. It is instructive to note, from NAFDAC’s data, that malaria prevalence in rural settings could be as high as 2.4 times that in urban setting, while the ratio between prevalence in children from the lowest social economic stratum to those from the highest could be as high as 7!
Other key determinants affecting the spread of malaria include the well- known fact that the use of the pesticide glyphosate (also implicated in cancer) weakens the immune systems of mosquitoes and render them more susceptible to infection by Plasmodium falciparum, thereby promoting spread of malaria. Similarly, the role of natural immunity in humans is also well-recognized. This is known to build up over the years for people living in malaria-endemic regions, and it effectively pushes the mortality burden squarely on children and pregnant women. There is also some measure of protection offered by the sickle cell trait (HbAS) as the premature breaking of erythrocytes truncates the lifecycle of the parasite.
Apart from the possibility of making ill-informed people to become complacent in their attitudes to traditional control methods, introduction of vaccines, if not carefully implemented, could drastically cut the level of funding and other resources available for these other more potent measures.
One major general outcry against vaccine-based solutions is the “Disconcerting over-dependence on foreign expertise and recommendations”. This robs Nigeria of what could have been at least some positive spin-offs in terms of development of human capacity which could have been useful in other sectors. Introducing the RTS,S in October 2021, WHO DG, Tedros Ghebreyesus had exulted: “This long-awaited malaria vaccine is a breakthrough for science. This is a vaccine developed in Africa by African scientists and we’re very proud,” It is not clear at all what he means by this, seeing that the vaccine was developed by the Walter Reed Army Institute of Research in the US and is marketed by British drugmaker, GlaxoSmithKline.
It is quite surprising that with our unenviable status as the malaria capital of the world, we cannot negotiate special prices for vaccines, not to talk of compelling the manufacturers to open factories here. It doesn’t require much imagination to perceive some positive correlation between Ghana’s being the 1st country to approve R21 and the decision of Serum Institute to open its sub-Sahara facility in Accra. And by the way, it is still a puzzle, the WHO’s Classification which deems Nigeria as NOT qualified to produce vaccines even for her own local use! Nigeria had actively produced vaccines for over 6 decades, until 1991 when a supposed upgrade grounded everything.
The peculiarity of vaccines is that, unlike drugs, they are to be administered to people who are not sick. Their justification is entirely premised on subjective risk:benefit analyses. The subject is conjectured as liable to be exposed to infection, is perceived to lack sufficient natural immunity to cope when so-infected, and envisaged to also lack adequate access to effective therapy to deal with the adverse outcome. Obviously, this framework cannot be easily generalized; and risk assessment for vaccine use must be personal to the individual.
It is a matter of historic fact that the currently available malaria vaccines were developed largely for military (US military to be specific) personnel who may need to be posted to malaria endemic regions. Hence they were not designed to prevent transmission; and their short-term efficacy of only a few months is generally adequate for this military need. To be frank, it would seem that the principal reason for presenting these vaccines for the use of babies in malaria endemic regions is largely to provide a market that would sustain the economics of mass production for the subjects they were actually designed to serve. [see Institute of Medicine. 2006. Battling Malaria: Strengthening the U.S. Military Malaria Vaccine Program. Washington, DC: The National Academies Press. https://doi.org/10.17226/11656].
In conclusion, while we may not castigate the malaria vaccines for whatever they are worth, it is important that we don’t confer them with silver-bullet status, which might jeopardize the effectiveness of other more potent tools for malaria management. As previously noted, people who wrongly assume their malaria worries are over with the receipt of the vaccine might get complacent in their compliance with other more fundamental measures bothering on environmental and lifestyle factors.
Even much more importantly, government must do nothing to coerce people into taking the product. There are good reasons to have fears this could be attempted. The PATH Technical Brief document lists a number of pre-conditions before a country will be “eligible” to buy their products. One of these is that such countries “will need to include the vaccine in both their national malaria strategic plan and their national immunization plan”. Other specific conditions call for the establishment of “joint immunization-malaria coordination mechanism” and also “Strong community engagement to ENSURE vaccine acceptance and resilient demand….” (page 7 - emphasis added).
All these look like subtle attempts to conflate malaria vaccines and other already accepted vaccines. In a previous article on the pentavalent vaccine, we cited WHO documents which confirm that significant health complications are introduced when multiple vaccines are co-administered together (simply for logistic reasons) rather than in the individual formats where they were originally developed.
All these may well explain the tardiness of the Federal Ministry of Health (FMoH) to submit an application for the RTS,S. For it looked evident that the announcement by the Ministry that it was sending in an application at the third window, was largely in response to growing vilification of the Ministry by the press who wondered why the Ministry was not joining in the excitement over the vaccine and had let two application windows fritter away.
It is worrisome to note that Nigerian reporters seem to find it easier contacting GAVI to inquire about Nigeria’s subscription to their product rather than asking the FMoH directly. Those who have read John Perkin’s Confession of an Economic Hitman might read this as GAVI actually reaching out to these local journalists to put pressure on the Honourable Minister! One may therefore better understand the reported response of the Minister when the press eventually reverted to him: “The Minister of Health could not be reached for comment. He did not take his calls and had yet to respond to a text message sent to him on the matter as of the time of filing this report.” https://punchng.com/nigeria-misses-malaria-vaccine-application-window/?amp
==============================================
Summary
This article is unavoidably a long-read. Apologies! It shows from hard records that the newly touted malaria vaccines were indeed developed for short-term visitors from the outside world to malaria-endemic zones (specifically military personnel and tourists). A strong market in sub-sahara Africa is however required to make their production economically viable! Notwithstanding that they very poorly meet the requirements to protect children in malaria-endemic regions such as Nigeria, we are reluctant to castigate them entirely. On the conditions that people (particularly the press!) are properly educated that these are no silver bullets; and government does not attempt to incorporate them into the list of essential vaccines to be vigorously recommended for the masses – as the manufacturers are already subtly demanding!
Joshua Ojo
Ile-Ife. 1st May, 2023